What is Vulvar Cancer
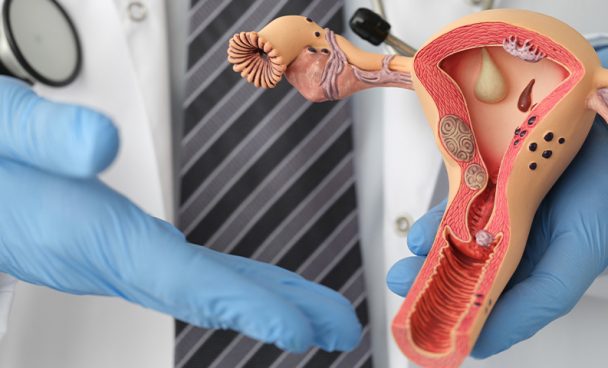
Vulvar cancer is a rare neoplasm (disordered proliferation of cells in the body) that occurs in the area around the vagina opening.
It corresponds to less than 1% of malignant tumors in women and it is responsible for 3% to 5% of malignant neoplasms of the female genital tract, with an annual incidence of 1 to 2 cases per 100,000 women in the USA. In Brazil, INCA (National Cancer Institute) has no estimates for vulvar cancer.
The average age at the moment of diagnosis is around 70 years old, with the incidence increasing as the years of life go by. Anyway, it is worth noting that the disease has apparently increased among young women, and in these cases the association with HPV is common.
In addition to advanced age, risk factors for vulvar cancer are:
- Lichen sclerosus – an inflammatory dermatologic disease, whose etiology is not fully clarified, although hormonal changes have been studied as one cause. Vulvar lichen sclerosus is usually associated with intense pruritus and the formation of a slightly pink or ivory-white papule, which may confluence to form plaques. Other related symptoms may be pain or burning. The potential for malignancy is about 4%;
- HPV (human papillomavirus) infection;
- Vaginal cancer;
- Cervical cancer;
- Smoking.
Subtypes of vulvar cancer
Vulva cancer is usually a skin cancer, with the following subtypes standing out:
- Squamous cell carcinoma – represents the majority of vulva cancer cases. The disease begins in the squamous cells (the main type of skin cell) and has three subtypes: keratinizing (most common type, affects older women and is not related to HPV), basaloid/verruca (less common, often affects younger women and with HPV) and verrucous carcinoma (rare and slow growing);
- Melanoma: represents about 6% of the vulva cancer cases and occurs from the cells that produce the pigment that gives color to the skin.
Symptoms and signs of vulvar cancer
The symptoms common to the several types of vulvar cancer are itching or discomfort, redness or change in the color of the vulval skin, appearance of unusual bumps (lumps) or flat sores (red or skin-colored). Sometimes these flat sores become squamous. In more advanced cases, bleeding may occur that is not associated with the normal menstrual period.
In melanoma, the color of the spot may be bluish-black or brown and it may be prominent, as well as having an asymmetric shape, irregular borders, a diameter greater than 6 mm, and potential changes in size, shape, and color over time.
Diagnosis of Vulvar Cancer
Vulva cancer is diagnosed by biopsy. First, the doctor diagnoses vulva cancer by taking a sample of the abnormal skin under local anesthesia and examining it in the biopsy. If the skin abnormalities are not well defined, dyes are applied to help determine where to collect the tissue sample. The doctor may also use a colposcope (an instrument with a binocular lens) to examine the surface of the vulva. This skin may prove to be just infected or irritated after the examination.
The doctor then determines the staging of the vulvar cancer (the stage it is at) based on its size, location, and whether or not it has spread to adjacent lymph nodes. This is known during surgery to remove the cancer. The stages range from I to IV, as follows:
- Stage I – cancer limited to the vulva or perineum (the area between the vaginal opening and the anus);
- Stage II – cancer has spread to adjacent tissues (lower part of the urethra and/or vagina or to the anus), but it has not reached the lymph nodes;
- Stage III – the cancer has spread to the adjacent lymph nodes, and it has or it has not reached the adjacent tissues;
- Stage IV – the cancer has spread further – for example, to the bladder, the upper vagina or urethra, the rectum, more distant lymph nodes, or outside the pelvis.
In addition, tests such as chest X-ray, CT scan, and MRI may be required.
Treatment
Treatment carried out in the early stages has better aesthetic, functional and healing results. The removal of all or part of the vulva is carried out in a procedure called vulvectomy. The adjacent lymph nodes are usually removed as well, or the doctor performs a sentinel lymph node dissection – the removal of the first lymph node that would be affected by the cancer.
In the case of more advanced vulvar cancer, radiation therapy enters the protocol, often jointly with chemotherapy, before vulvectomy. This protocol can reduce the size of very large tumors, making them easier to remove later.
Prevention
Prevention of vulva cancer is possible with attention to body signs and by avoiding its risk factors. It is recommended:
- Going for an appointment with a gynecologist doctor when noticing changes in the vulva region. It is worth emphasizing: be aware, not all pruritus (itching) is related to vulvar candidiasis;
- Do not smoke;
- Get vaccinated against HPV.